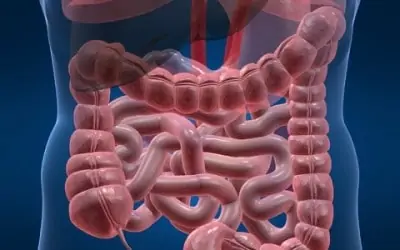
Acute appendicitis is a very common emergency, presenting with equal likelihood at any stage in one’s life. The appendix is a vestigial organ, and has no function in humans. Arising from the very beginning of the large intestine (colon), it can become blocked by fecal matter, preventing drainage, leading to bacterial overgrowth and the clinical presentation of appendicitis.
The advances in surgery at the end of the nineteenth century, and the subsequent improvements in medical care throughout the twentieth century, have made what once was an often-fatal illness a disease that usually can be cured rather easily. Today, appendicitis is a very, very rare cause of death.
While on rare occasion appendicitis may subside spontaneously, the treatment almost universally is surgical – an appendectomy - removing the appendix. If the disease is diagnosed promptly, and the appendix removed before it ruptures, the usual hospital stay is brief and patients are back to full activities within a week to ten days. However, if the appendix ruptures and peritonitis (inflammation of the abdominal cavity), abscess, or other complications develop, the illness may be quite prolonged.
Virtually every surgeon, emergency room physician, primary care doctor, etc., has “missed” the diagnosis of appendicitis at some time during his or her career. This is not necessarily below the standard of care; detecting appendicitis is often a quite challenging problem. Even with today’s improved diagnostic acumen, the number of instances when appendicitis is not promptly diagnosed, leading to rupture, peritonitis, abscess, etc., is decreasing, there still are occasions when appendicitis confuses patient and physician alike. The body’s natural defenses “wall off” an inflamed organ, and indeed pain and other symptoms often will improve transiently.
It thus is important that a patient who presents with abdominal pain and is felt not likely to have appendicitis be advised to follow-up promptly if symptoms do not completely resolve. It likewise is important for emergency room and other physicians to have a great degree of suspicion when a patient returns with the same or similar complaints. Common diseases present in somewhat unusual fashion far more often than do rare problems.
Diagnosing Acute Appendicitis
Appendicitis classically presents with the sudden development of severe, steady abdominal pain. The discomfort starts about the umbilicus, and then migrates to the right lower abdomen. Nausea and/or vomiting follow. The bowels stop functioning, and appetite is lost. The white blood cell count and temperature rise. Secondary signs of infection – generalized toxicity – worsen as the disease progresses.
Although this “classic presentation” is most common, the symptoms vary widely, ranging from someone who suddenly becomes deathly ill to a discomfort that seems insignificant until it has gone on for several days. Not everyone has the migrating pain; not everyone is nauseated or vomits; some people continue to eat without problems. Bowel movements may continue, or there may even be diarrhea. In some, the white count remains normal.
Typical findings upon physical examination include tenderness in the right lower abdomen, often with some spasm of the muscles in the abdominal wall in the area. Bowel sounds often are quiet; there may be “rebound” or “percussion” tenderness: in other words, jiggling the abdomen aggravates the pain. Patients often complain that while driving to the emergency room or doctor’s office going over a bump aggravates the discomfort.
With the key to treatment of appendicitis being early diagnosis, it remains an art for the surgeon, in particular, and other physicians to try to distinguish appendicitis from other causes of abdominal pain, nausea, vomiting, etc. Clinical acumen remains the number one diagnostic tool. Because of the fear of “missing” the diagnosis and possibly allowing the appendix to rupture, it was widely accepted for many years that one would operate in uncertain instances, accepting that the appendix might be normal in as high as twenty percent of operations. Recent advances have reduced this rate of negative exploration, but there always will be uncertainty; operation often is the safest and most conservative option.
Through the years physicians have tried to improve diagnostic accuracy using various X-ray and other imaging studies. Plain X-rays of the abdomen are usually unproductive. In the 1980’s, ultrasonography was advocated to help make the diagnosis; unfortunately, it is not very accurate, but remains quite helpful in young women in trying to distinguish gynecological problems from appendicitis. If the appendix is visible on ultrasonography, the patient likely has appendicitis, but most diseased appendices are not identified.
Computerized axial tomography, or CT Scanning, has become the most widely used and important imaging technique to help identify patients with acute appendicitis, perhaps to the point where it is overutlilized. [It is this surgeon’s opinion that in the classic presentation of appendicitis, especially in an otherwise healthy young male, there is little need for fancy imaging studies; one can proceed promptly to operation without the expense of additional studies.] CT scanning typically will identify an inflamed appendix. The radiologist often will describe the “dirty fat” of inflammation about the organ. The CT may identify other problems, and thus help in the differential diagnosis. Accuracy rates in diagnosing appendicitis of as high as 98 % have been reported.
Confusion in the diagnosis (and the majority of the cases in which the surgeon finds a normal appendix) is most common in young, menstruating women. Diseases of the ovaries, Fallopian tubes, and uterus are actually more common than appendicitis. Problems such as a ruptured or twisted ovarian cysts, ectopic pregnancies, and pelvic infections can mimic appendicitis exactly. In addition to the imaging studies, the laparoscope has been particularly beneficial in this setting. It readily allows visualization of the pelvic organs and appendix through small incisions, permitting accurate diagnosis and treatment of the problem identified.
Surgical Treatment
Appendectomy was first performed in the late 1800’s. There is little controversy concerning the techniques used in open surgery. Usually a small incision is made in the right lower abdomen, the muscles of the abdominal wall stretched apart, the abdominal cavity entered and the appendix removed.
With the development of minimally invasive surgery, it has become increasingly attractive to remove the appendix using laparoscopic techniques. However, unlike cholecystectomy (gall bladder removal), in which there was a dramatic decrease in postoperative pain and hospital stay with the development of the laparoscopic approach, a dramatic shift in recovery time has not occurred with laparoscopic appendectomy. The reason likely is that the diseases are different. When removed, the appendix typically is acutely inflamed and infected, and antibiotics and other treatment are needed to resolve the infection. Antibiotic therapy is usually initiated before surgery and is required postoperatively for a varying time, depending on the degree of infection.
Laparoscopic appendectomy does seem to have some advantages, and increasing numbers of appendectomies are being done laparoscopically. Wound infection rates may be a bit lower, and time to return to work averages a day or two sooner. Some studies, however, suggest a higher rate of late intra-abdominal infections with laparoscopic surgery as compared to traditional open techniques.
Not all appendicices can be removed laparoscopically. What has become clear is that the decision to attempt laparoscopic vs. open removal has to be made on a case-by-case basis. Often it may involve an initial laparoscopic step for diagnosis and then making a conventional incision (perhaps a bit smaller since the location of the appendix may be pin-pointed) for appendix removal.
The appendix is sometimes removed incidentally during an operation for another problem. While this has decreased in popularity among general surgeons and gynecologists, it is important for patients undergoing abdominal operations to know whether or not the appendix was removed. When the operation is done for suspected appendicitis, and then the appendix is found to be normal, and no alternative disease or contradiction to appendectomy is identified, it is usual practice to remove the appendix to avoid future confusion. Thus every patient needs to know the surgical findings and the operation accomplished, as well as the pathologist’s report—does it confirm the surgeon’s diagnosis of acute appendicitis? It is quite acceptable to remove a normal appendix; it is not acceptable for the patient not to know the full nature of the illness.
