SUMMARY: (RHABDOMYOLYSIS) is a syndrome resulting from destruction of striate(skeletal) muscle cells with leakage of muscle intracellular toxins into the bloodstream, characterized by few symptoms, the most common being myalgia (muscle aches and cramps) and dark urine, and few sentinel laboratory findings, the most specific being a positive dipstick test for blood with few rbcs seen on microscopy, and elevated CK (creatine kinas ) in the blood. It occurs in Trauma situations, such as Crush injuries, where large quantities of muscle are destroyed. More commonly, it develops in situations where moderate to severe exercise occurs, particularly in hot humid climates, in de-conditioned individuals. Renal failure, cardiac arrhythmias, coma and death may develop.
Dehydration is especially conducive to serious complication of Rhabdomyolysis. Toxins, illnesses, genetic defects (regarding ATP production) and electrolyte imbalance, are common environments where this syndrome often occurs.
First and foremost is the ability to suspect rhabdomyolysis in the appropriate clinical settings.
Treatment consists of treatment of the underlying condition, removal of the offending medication or toxin, rest, rehydration, and alkalinazation of the urine. Renal dialysis and treatment of Hyperkalemia may become necessary.)
When skeletal muscle is irritated or inflamed it often becomes sore and tender and the muscles ache. This MYALGIA can occur in a number of conditions. Viral Influenza is one of the more common causes of generalized muscle aches or myalgia. Certain medications, such as Statins, which are used for Hypercholesteremia, are occasionally associated with the onset of myalgia. Myalgia is most often transient, especially in it’s most common form, which is over exercise. It may resolve once the underlying illness has run it’s course, or the offending medication is stopped or simply by rest and hydration.
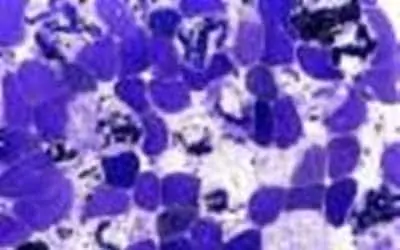
When myalgia intensifies, it involves the death and destruction of the skeletal muscle cells, called myo-cytes, then MYOSITIS develops. In this instance, substances, which belong within the cytoplasm of the cell, leak out into the blood. Such substances as creatine, myoglobin, aldolase, potassium, and lactate dehydrogenase are extruded into the blood stream. Myoglobin is the form of Hemoglobin found in muscle cells which transfers Oxygen and Carbon Dioxide. Myositis is characterized as exquisite tenderness of the affected muscles and the person may not be able to tolerate even the slightest pressure. The muscles may become swollen and boggy in consistency.
If the myositis is allowed to intensify, then irreversible damage may occur, generally from the muscle swelling, which, in turn, causes compression of vessels and nerves and results in massive dissolution of significant quantities of muscle. Dissolution of the myo-cytes and the subsequent release of large quantities of toxic intracellular components into the systemic circulation and the end organ consequences constitute the syndrome of RHABDOMYOLYSIS.
RHABDOMYOLYSIS may involve many organ systems, but the life threatening consequences are related to electrolyte abnormalities, i.e., acute hyperkalemia, hypocalcemia, and acute renal failure. When muscle is deprived of nutrition and circulation, intracellular-free Calcium is increased to critical levels and this triggers several degradative processes culminating in muscle cell death and in extravasation of intracellular toxins into the systemic circulation. The contraction of the extra cellular fluid volume appears to be the principal determinant of the renal toxicity of myoglobin.
Signs and Symptoms
The symptoms of Rhabdomyolysis are nonspecific and consist of an increase in ventilation, in an effort to blow off acidic CO2, and central nervous system function depression, manifesting itself as headache, lethargy, stupor and even coma, as well as severe unexplained muscle pain, cramps and weakness. The muscles may be swollen and tender. The most commonly affected muscles are those utilized in exercise. Fever may be present, especially if associated with infections. The extremities will demonstrate painful decreased range of motion. However, some patients are asymptomatic, necessitating the laboratory workup to suggest the diagnosis. So, it’s important that physician must maintain a high index of suspicion, which generally is tipped off by appropriate history and physical in the clinical situation, reflecting one of the many causes of Rhabdomyolysis.
Laboratory elevation of the CK (Creatine Kinase) is a key to the diagnosis, and is the most sensitive indicator. The CK is usually 5 times or more greater than the normal level and can be greater than 100,000 IU/L. Exercise to near exhaustion, is associated with a CK rise of only about 10,000 IU/L. Still, there is poor correlation between CK elevations and the morphologic degree of muscle damage. Urinalysis, initiated because the urine will darken (often the first clue) with the increased excretion of myoglobin, will demonstrate a positive test for hemoglobin, but the microscopic exam will show only a few red blood cells, suggesting Rhabdomyolysis. Microscopic urine exam may demonstrate “Muddy casts”, which re diagnostic of myoglobin or hemoglobin in the renal tubular fluid.
Once suspected, from the clinical symptoms, the clinical setting, especially the history of the illness, and the initial lab. tests, then measuring the Myoglobin in the urine and serum may confirm the diagnosis. Once the renal threshold for myoglobin is reached, myoglobin is cleared at 75 per cent of the glomerular filtration rate. If there is marked muscle breakdown, the serum myoglobin lever may be elevated.
Abnormal electrolyte findings may trigger off the premonition suggesting Rhabdomyolysis, by he presence of Hypernatremia, Hyperkalemia, Hyperuricemia (secondary to enhanced release of purine precursors), and Lactic acidosis (secondary to glycogen depletion and anaerobic metabolism).
As the renal status deteriorates, the urine output may fall suggesting oliguric renal failure.
CAUSES OF RHABDOMYOLYSIS
Traumatic damage to large quantities of muscle was recognized during Crush Injuries in the Second World War and the diagnosis of Rhabdomyolysis was anticipated and recognized frequently.
Since then, Non-traumatic causes of Rhabdomyolysis are now recognized as being more frequent than the traumatic causes. It may occur after moderate to severe exercise in otherwise healthy people. This is reported to occur among young unconditioned military recruits, particularly in hot and humid military training. The heat generated during exercises encourages shunting of the blood to the surface for heat dissipation, depriving the kidneys and gastrointestinal tract of blood. This causes deterioration of the gut wall, allowing invasion of intestinal bacteria and bacterial toxins into the blood stream. This transient septicemia in the environment of a contracted body fluid volume can lead to myoglobin-induced renal failure.
Some genetic enzyme deficient conditions are associated with muscle necrosis even after minimal exercise.
Chronic Alcoholics are particularly susceptible to Rhabdomyolysis in certain situations. After binge drinking, there are significant electrolyte concentration changes in he muscle cells causes by direct injury from alcohol. These people often have deficiencies in potassium and phosphorus homeostasis, as well as easy susceptibility to infection, which may intensify the toxic effects of alcohol. In cirrhosis of the liver, phosphorus and potassium are shifted from the blood into the intracellular compartment, rendering the alcoholic more susceptible to rhabdomyolysis.
Recently Rhabdomyolysis has been associated with viral , bacterial and rickettsial Infections. It appears that the these organisms may attack the muscle directly or may lead to muscle-specific toxin generation. It occurs most commonly with influenza virus type A and B. It is seen in HIV patients as a sequelae to acute myositis, especially as part of the febrile illness that precedes seroconversion after infection. Certain bacteria, such as Lenionella species, Streptococcus species, Tularensis and Salmonella species have been incriminated. Several reports confirm the association between Q fever and Rocky Mountain spotted fever, rickettsial infections, to Rhabdomyolysis.
Chronic electrolyte imbalances, such as hypokalemaia and hypophophatemia may precipitate rhabdomyolysis. This has been reported also, in patients who drink excessive quantities of fluid, especially water, lowering their sodium (hyponatremia). Low potassium conditions which may potentiate the possibility of Rhabdomyolysis are seen with chronic administration of long-acting thiazide diuretics, certain antibiotics, and even ingestion of mineral corticoid-like substances, such as licorice. Hypomagnesemia, and even hypernatremia have been incriminated. Diabetic ketoacidosis has been reported to cause Rhabdomyolysis.
Heatstroke has been incriminated, as has hypothermia. This is especially susceptible when the addition of exercise is added. Once again, this appears to be do to shifts in intracellular Calcium and Phosphorus.
Miscellaneous Causes include Cocaine abuse, carbon monoxide poisoning, neuroleptic malignant syndrome, and prolonged coma in a fixed position (Saturday night Palsy).
Another classification of Rhabdomyolysis divides the types into 1.) Pure exertional, 2.) Exertion in those with genetic enzyme deficiencies, and 3.) Exertion in Nonhereditary forms. The first type is the typical heavy exertional type. The second category occurs in those individuals, who have defects in the pathways by which ATP is generated. These defects in the environment of exercise will contribute to Rhabdomyolysis. The third category includes those precipitating factors such as drugs, toxins, or infections, in which, the addition of exercise will cause muscle breakdown. Therefore exercise in patients who are alcoholic or have ingested cocaine (especially if they have an associated potassium and phosphate deficiency) places them at exceptional risk for Rhabdomyolysis.
DIFFERENTIAL DIAGNOSIS
The major physical clue to Rhabdomyolysis is the presence of painful, aching, and tender muscles. But this can also occur in primary muscular disorders, such as: Polymyositis, dermatomyositis, rheumatoid arthritis, fibrositis, polymyalgia rheumaica, tendonitis, localized infection and even with some medications (steroids, diuretics).
The other major clue, i.e., dark brown urine, can be seen in: hemoglobinuria, porphyria, uorbilinogen, medications (nitrofurantoin, priqmaquine, metronidazole, rifampin).
KIDNEY FAILURE
Renal failure appears to occur form the direct toxic effects of the excessive myoglobin. Myoglobin’s toxic effects appear to be enhanced by a diminution in extra cellular fluid volume, which is especially seen in trauma, where large volumes of fluid may extravasate into the lower extremities, resulting in severe ECF volume contraction. Renal failure is one of the most common cause of death in this condition.
Myoglobin, through it’s metabolites, is directly cyto-toxic to the renal cells. The production of oxygen and non-oxygen free radicals, because of the excess of free iron, lead to oxidant stress and injury to the renal cells. There is evidence that the alterations in the intracellular glutathione may contribute to the pathogenesis of pigment-induced renal failure.
Myohemoglobin may form tubular casts in the renal tubules, especially in an acid urine, which, once formed, may cause intra-tubular obstruction and increase in pressure and resultant diminished glomerular filtration rate, aggravating the already ongoing kidney damage.
TREATMENT
Irrespective of the etiology of the breakdown of the muscle cells, Rhabdomyolysis is potentiated if the extra cellular fluid volume is contracted, such that the urine output is diminished. So, the first and most important goal in treatment is to increase the urine output. This is most expeditiously done by giving IV normal saline, from 4 to 6 liters within the first 24 hrs.
Since the nephrotoxic effects of myoglobin are potentiated in an acidic urine setting, giving of Bicarbonate to alkalinize the urine is very beneficial. Maintenance of the urine pH greater than ki6 prevents disassociation of the myoglobin.
Since diuresis of the excessive Myoglobin is one of the goals, the giving of an osmotic diuretic such as Mannitol is very helpful. Lasix also can be given for it, fast diuretic action and it’s acidification of the urine.
Treatment of the underlying condition, such as a Compartment Syndrome, where increased intercompartmental pressure is elevated with deprivation of blood flow and death of tissue, by a fasciotomy is crucial.
Treatment is continued until the urine dipstick is negative for blood, creatinine is normal and the other laboratory tests indicative of Rhabdomyolysis are returned to normal.
COMPLICATIONS
Acute Renal Failure--This is the most serious complication, and may require renal dialysis, hopefully for the short haul, only.
Cardiac Arrhythmias-- Because of the electrolyte imbalances commonly encountered, the heart muscle may become irritable and potentially fatal rhythms may ensue. Checking for and treating these imbalances are mandatory.
Disseminated Intravascular Coagulopathy (DIC)--This is a condition combining bleeding and excessive clotting simultaneously, resulting in death of vital organs. It must be anticipated and Cardiomyopathy and respiratory failure may ensue.
PREVENTION
Since excessive exercise is the more common culprit in the enviroment of predisposing factors, such as Substance Abuse, genetic enzymatic defects, or de-conditioning, it is wise to recommend gradual increase in exercise activity, particularly in the proper temperature and humidity, and to encourage adequate hydration.
References:
- Bobby Adcock;Rhabdomyolysis: XIV Musculoskeletal/Connective Tissue Diseases);
- P. Visweswaran M.D., J. Guntupalli, M.D.;Rhabdomyolysis; Critical Care Clinics, Vol 15. No. 2. April 1999, (Pg. 415-427).
- Juha P. Kokko:Rhabdomyolysis: IX Critical Care Medicine; Pg. 522-525;
