According to the Glascow Coma Scale, a moderate TBI is defined as a GCS score of between 9 and 12. According to the Abbreviated Injury Scale, (AIS), an anatomically based, consensus derived global severity scoring system, a moderate traumatic brain injury is defined as one scoring an AIS of 3-4.
Some health care providers use a combination of the clinical picture, GCS, AIS and neuroimaging to help define or distinguish between an mTBI and a moderate TBI or a severe TBI and a moderate TBI.
It is generally understood that the more life threatening the head injury is to the patient, the more severe the TBI is thought to be. Thus, there is some gray area among health care providers in determining where a mild TBI stops and a moderate TBI begins and where a moderate TBI stops and a severe TBI begins.
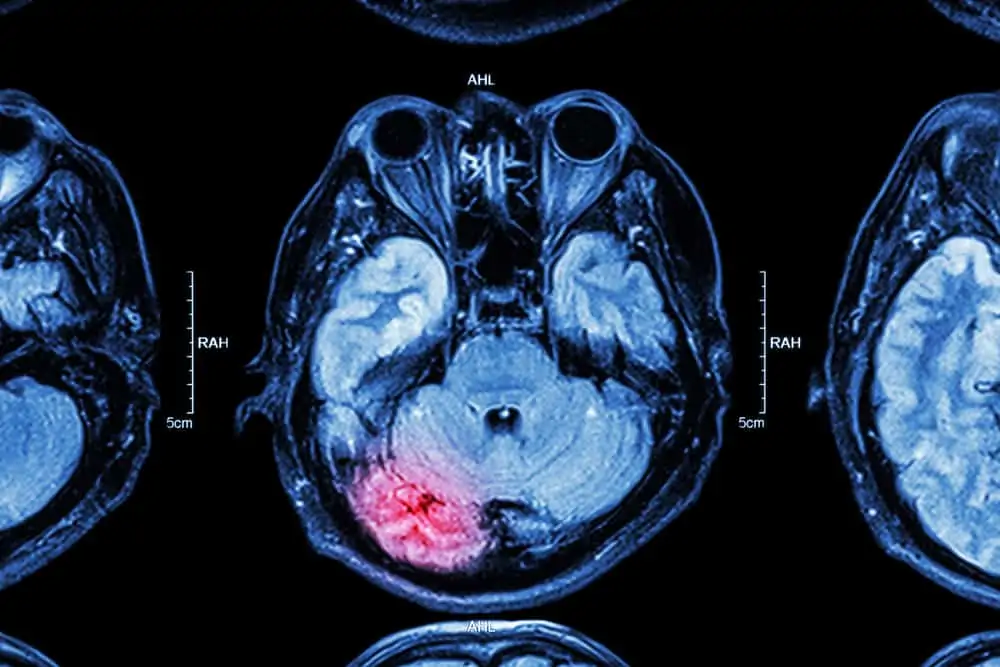
Many simply classify a moderate TBI as a head trauma causing a loss of consciousness less than 30 minutes or an alteration in the mental state at the time of injury, plus a significant finding (hematoma or bleeding) shown on neuroimaging.
Others may use a more basic definition of moderate TBI as that when a person experiences changes in brain function for longer than a few minutes following trauma when the symptoms do not go away or may even get worse.
